Discharge is a broad term and is made up of skin cells, bacteria, mucus and fluid produced by the vagina and cervix. Its role is to protect the vaginal and urinary tract against infections and also acts as a lubricant to stop friction and irritation
What does ‘normal’ discharge look like?
All women will have discharge, which is normal, this is referred to as ‘physiological’ discharge. Physiological discharge is either clear or white and will change in texture throughout your cycle and come from your cervix. It will be thick and sticky throughout most of your cycle but will become thinner, clearer and stretchier around the time of ovulation, like the texture of egg white. Sometimes when the discharge dries, it may appear yellow on your underwear (1,2).
The amount of discharge may also vary throughout your cycle, often, you may notice more discharge before you are due to ovulate around the middle of your cycle. Daily vaginal discharge (about 1-4ml every 24 hours) is pretty normal and healthy
Typically, vaginal discharge will not have a particular smell, however, you may recognise what is normal for you. Changes in this smell may represent an infection for example.
Please do note, that if you take hormonal contraception, the ‘cycle’ of change in your discharge will be disrupted and will likely not follow this pattern (2). Similarly, women who are post-menopausal typically have less discharge as a result of lower levels of oestrogen.
So if my discharge is always changing – how do I spot signs of abnormal discharge?
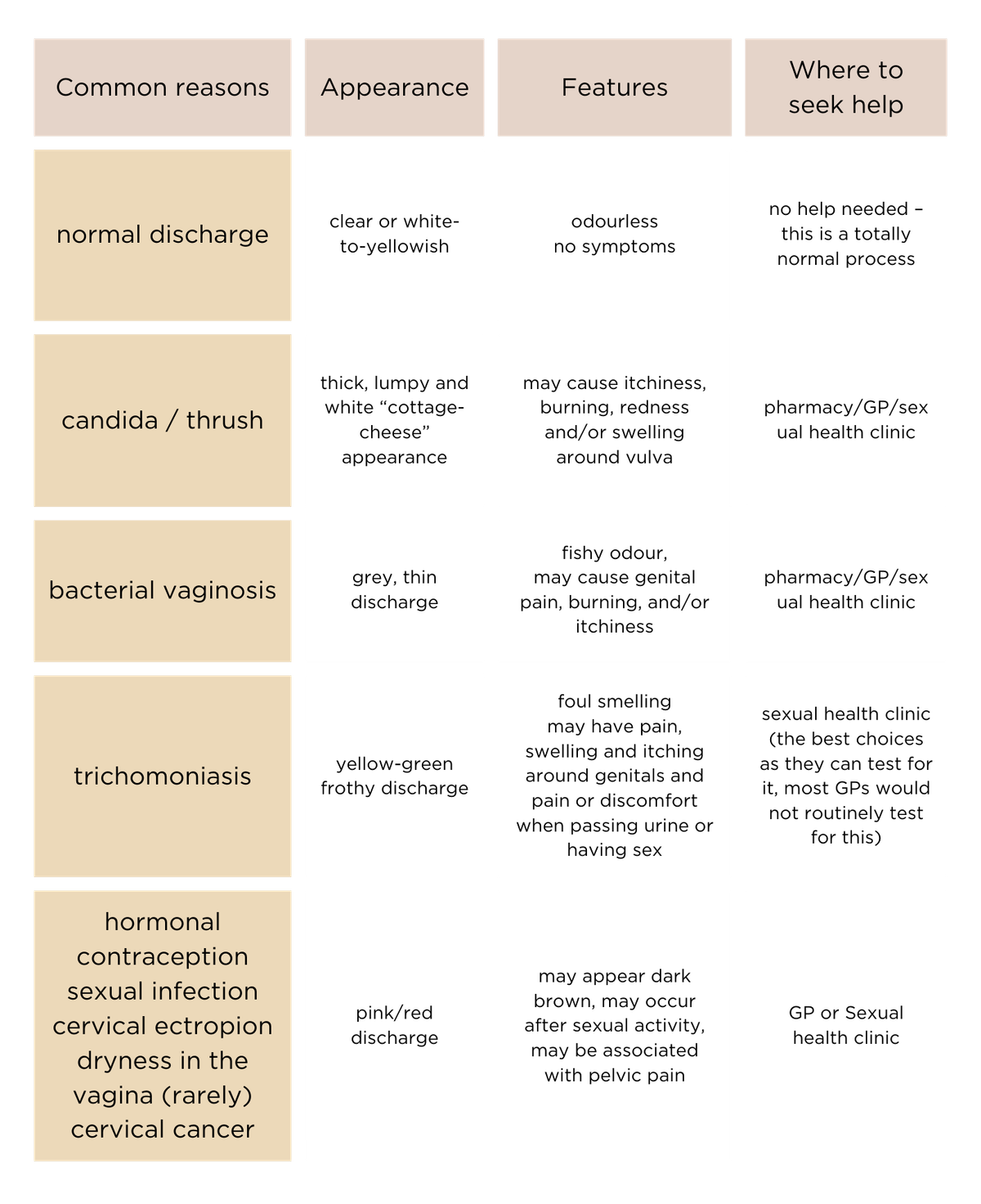
The abnormal discharge could be caused by a number of things, including an overgrowth of yeast (known as candida or thrush), bacterial vaginosis (or BV), Sexually Transmitted Infections (STIs), or less commonly, cervical cancer.
Candida/thrush
Vaginal thrush (A.K.A. vulvovaginal candidiasis) is caused by an overgrowth of a fungus called candida in the vagina. Small numbers of Candida commonly live on the skin and around the vaginal area and cause no issues. However certain changes or conditions can cause candida to multiply, leading to the classic symptoms of thrush. That is; “cottage cheese” discharge, itchiness, burning, and in some cases redness around the vulva. This can be treated by a treatment which is available over the counter from the pharmacy, from your GP or your sexual health clinic.
Bacterial vaginosis (BV)
If you notice a fishy odour, with a grey, thin discharge, this may represent a condition called Bacterial Vaginosis or BV (5). BV is caused by an imbalance of bacteria in the vagina. This often occurs as a result of over-washing e.g. vaginal douching, new soaps or a new sexual partner. BV is not a sexually transmitted infection, but more caused by the change in the types of bacteria present in the vagina. The vagina is ‘self-cleaning’, and hence over-cleaning the vagina can lead to other issues such as BV. BV can also cause a burning pain in the vagina. There are tests available over the counter which can help to test for BV. A sexual health clinic or your GP would also be able to help with this, although most cases are diagnosed based on clinical history. Treatment should ensure that patients do not overwash, as this will delay the recovery, but can be hard as patients are often conscious of a smell. Antibiotics, both in tablet and gel forms can be used to treat BV.
Sexually transmitted infection
Sexual infection can cause changes in vaginal discharge, as well as other symptoms such as discomfort in your pelvis, pain during sex, unscheduled bleeding (in between your periods or after sex) as well as urinary symptoms. Green and frothy discharge can represent a specific sexual infection called Trichomoniasis (4), which is often best diagnosed at a sexual health clinic. If you do find that you have a sexual infection, it is important to have treatment and ensure that your partner(s) have been treated. If you have further sexual intercourse without both parties being treated, then there is a high chance of reinfection and your symptoms will return and may become more severe.
Pink discharge
If you ever notice a pink stain in your discharge, this would normally represent blood (5). If this happens outside of your period, you may need to see a doctor. Any bleeding in between your periods or after sex may need investigation. Hormonal contraception may impact your bleeding pattern, and some types of contraception cause spotting which may show as pink discharge. Occasionally, when some women ovulate they have pink discharge. If you have irritation in your vagina, this can also lead to pink discharge e.g. if you are around the time of menopause, or had irritation from sexual activity. Bleeding can come from the womb, the cervix, the vagina or surrounding skin. It is important to ensure that your smear tests are up to date, however, if you have evidence of bleeding in between your cycles, the doctor may need to examine your cervix again. One common condition is called cervical ectropion, where the cells on the cervix are more prone to bleeding, this is often not a problem but will require an examination. If your doctor suspects bleeding is coming from your womb abnormally, they may request other tests such as an ultrasound.
See a GP or go to a sexual health clinic if you notice:
- Changes in smell e.g fishy
- Changes in colour e.g. green, brown, grey
- Changes in consistency e.g. cottage cheese or frothy
- Changes in volume i.e you produce more discharge than usual
- Any associated symptoms i.e ulcers, bleeding, pain, redness
Should I take a probiotic?
Probiotics are often considered for your gut microbiome, but in fact, your vagina has its own microbiome which probiotics can impact. Lactobacilli are the most well-researched strains of probiotics which are thought to improve the bacterial balance in the vagina (6,7). These can also be found in live yoghurts.
Probiotics need to be stored in specific conditions and taken at a recommended dose to try and restore the balance in the vagina with the aim of reducing recurrence of vaginal infection.
Some people may find it useful to take probiotics whilst taking a course of antibiotics, to help to prevent conditions such as thrush from occurring, particularly if this is something you are prone to.
The evidence for probiotics is not conclusive, but as an adjuvant therapy, it can improve the rates of short-term cure, although there is no clinical evidence for long-term benefit (6). There are also preparations of vaginal probiotics which are available (7).
Summary
Everyone’s vaginal discharge is different and can be impacted by a variety of factors. If you notice a change in your discharge or ever have any signs of bleeding which is not during your period, please consult a healthcare professional. Rarely, abnormal discharge can be caused by an issue with your cervix, so it’s important to stay up to date with your smear tests.